
A 39-year-old patient was admitted in a critical condition (with a right parietal hematoma) to Department of Neurosurgery No. 3 of Polenov Neurosurgical Institute (branch of Almazov Centre) specializing in the treatment of patients with complex cerebrovascular conditions.
The patient presented with a depressed level of consciousness, troubled speech, weakness in the left extremities. Cerebral angiography revealed a rare cerebrovascular disorder – a polyafferent arteriosinus fistula characterized by multiple arterial branches extending from both extracranial and intracranial arteries draining blood into the sinus system of the brain.
Apart from this, MRI showed that the patient had multiple congenital vascular malformations – cerebral cavernous malformations, and one of these (located in the right parietal lobe) was the cause of intracranial hemorrhage.
The patient previously received radiosurgical treatment for cavernous malformation as well as a course of conservative therapy for a traumatic brain injury as a result of a seizure. No surgery for cavernoma was performed.
The medical team together with Director of the Institute Konstantin Samochernykh planned a staged treatment combining both intravascular technique and microsurgical procedure.
The open surgery was performed by Board Certified Neurosurgeon of Department of Neurosurgery No. 3, Saidakhmed Radjabov.
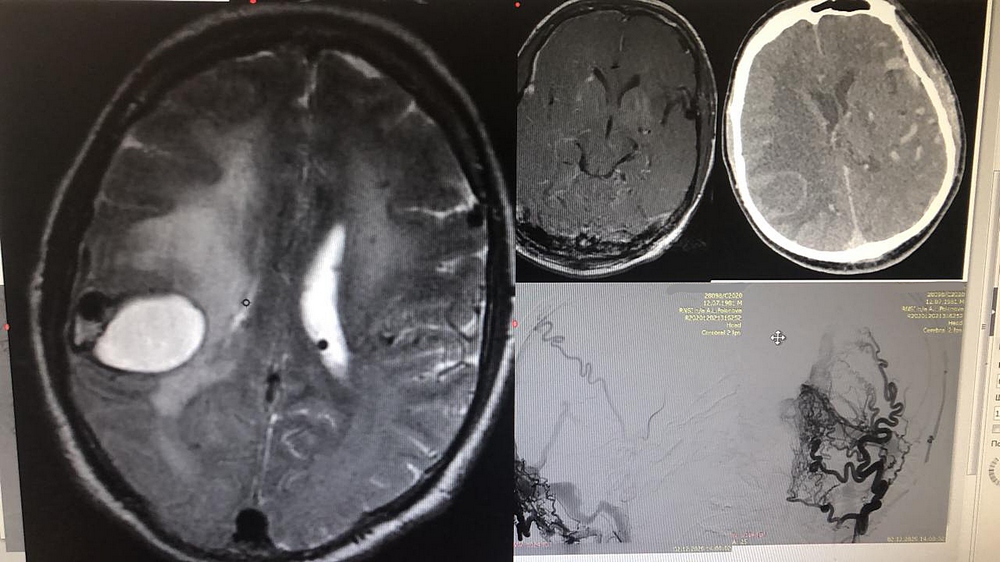
Right parietal intracerebral hematoma. Abnormal vasculature in the fistula
The surgical removal of intracerebral hematoma and cavernous malformation of the right parietal lobe was associated with an extremely high risk of massive bleeding due to the functioning arteriosinus fistula. Because of its volume, the hematoma had to be removed quickly.
In order to minimize the risk of bleeding, the first stage included intravascular partial embolization of the arteriosinus fistula with a special polymer to reduce blood flow in the abnormal vessels. The second stage was the removal of the cavernoma and hematoma of the right parietal lobe using a modern neuronavigation technique, a microscope and intraoperative neurological monitoring system.
Subsequently, the patient underwent two more intravascular procedures enabling to completely exclude the abnormal vasculature from the blood flow, normalize cerebral blood flow and eliminate the risks of repeated intracranial hemorrhages.
At the first stage, the treatment was conducted by Board Certified Neurosurgeon Larisa Rozhchenko. Afterwards, the patient was treated by neurosurgeons Andrey Petrov and Vasily Bobinov.
After treatment, the patient showed a good recovery: he regained consciousness without speech impairments and motor impairments of the left extremities significantly decreased. He will be discharged after rehabilitation.
Every year, the surgeons of the department perform hundreds of intravascular and microsurgical procedures of various complexity. A personalized approach to each patient with complex cerebrovascular diseases helps not only correctly plan the treatment but also significantly increases the patient's rehabilitation potential.

