 A pregnant woman was admitted to the Perinatal Centre at Almazov Centre for her scheduled delivery as she suffered from thrombocytopenia, a blood disorder requiring medical observation and, if necessary measures to prevent bleeding. The screening ultrasound did not reveal any fetal abnormality. The woman gave birth on time and without complications. However, as soon as the baby girl was born, doctors noticed her huge belly. The ultrasound scan was performed on the first day and revealed a large solid mass in the liver occupying almost half of the abdominal cavity.
A pregnant woman was admitted to the Perinatal Centre at Almazov Centre for her scheduled delivery as she suffered from thrombocytopenia, a blood disorder requiring medical observation and, if necessary measures to prevent bleeding. The screening ultrasound did not reveal any fetal abnormality. The woman gave birth on time and without complications. However, as soon as the baby girl was born, doctors noticed her huge belly. The ultrasound scan was performed on the first day and revealed a large solid mass in the liver occupying almost half of the abdominal cavity.
“Conservative methods failed to stop bleeding. The child's hemoglobin rapidly decreased, the abdominal size progressively increased. Within three hours, the situation became critical and required an emergency surgery,” says Dmitry Petrov, Chief of the NICU. During the surgery, the bleeding was stopped, its source was the rupture of the spleen due to the strongest pressure from the huge liver. Due to massive damage, the spleen had to be removed. During the procedure, tumor material was taken for histological examination.
“Histological analysis confirmed our worst fears. We dealt with hepatoblastoma, a malignant liver tumor that develops from an embryonic pluripotent anlage,” recalls the operating surgeon, chief of the Pediatric Surgery Department Anna Sukhotskaya.
The tactics of further treatment was based on the existing standards of medical care for children with this disease and included five courses of chemotherapy followed by surgical treatment.
“The aim of chemotherapy is to reduce the volume of the tumor in order to advance to the next stage of treatment – its removal. It is a rare case to make an accurate diagnosis at such an early stage, so treatment was started already on the 19th day of the girl's life,” says Chief of the Department of Chemotherapy for Oncohematological Diseases and Bone Marrow Transplantation for Children Yulia Dinikina.
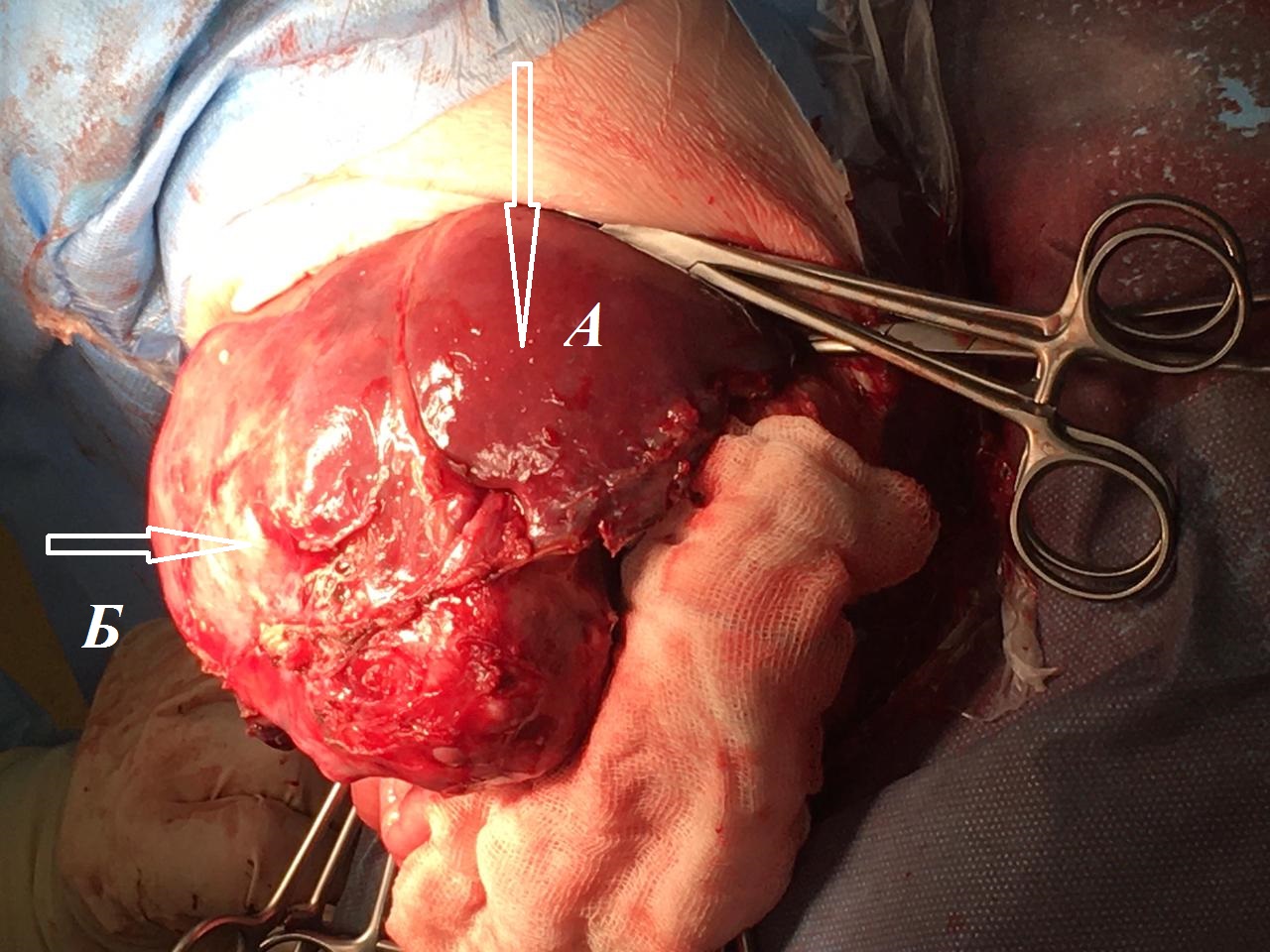
А — normal liver, Б — tumor
At the age of three months, the patient underwent a radical surgery – right hemihepatectomy (removal of the right half of the liver). The doctors used the Cell Saver autotransfusion device intended to recover blood shed during surgery collect the patient's own blood and immediately reinfuse it intraoperatively. “During the surgery, a histological analysis of the lymph nodes was performed, which revealed that they were not affected by cancer cells due to the successful chemotherapy. The success of the surgery largely depended on the efforts of the anesthesiologists,” comments the operating surgeon, head of the Surgical Diseases Department, Prof. Vladimir Bairov.
The surgical treatment was followed by two more courses of chemotherapy indicated for hepatoblastoma. A month and a half later, complete remission was confirmed. The patient's prognosis is favorable but doctors recommend regular check-ups and tumor marker monitoring. The success of the treatment was achieved by the combined efforts of various specialists at Almazov Centre: surgeons, oncologists, intensivists, pathologists.
