
The first symptom of the disease experienced by the 15-year-old boy from Murmansk was a sudden epileptic seizure.
“During a break at school, I stopped understanding what my classmates were saying – I heard that they were addressing me, but I couldn’t understand the words. And in a few moments I remember that I woke up, I was lying and everyone gathered around me…,” the boy recalls that day.
The boy underwent an MRI that showed a brain tumor measuring about three centimeters in diameter located at the junction of temporal and parietal lobes, the speech region controlling speech comprehension, the ability to combine words into complex phrases, recognize and name objects.
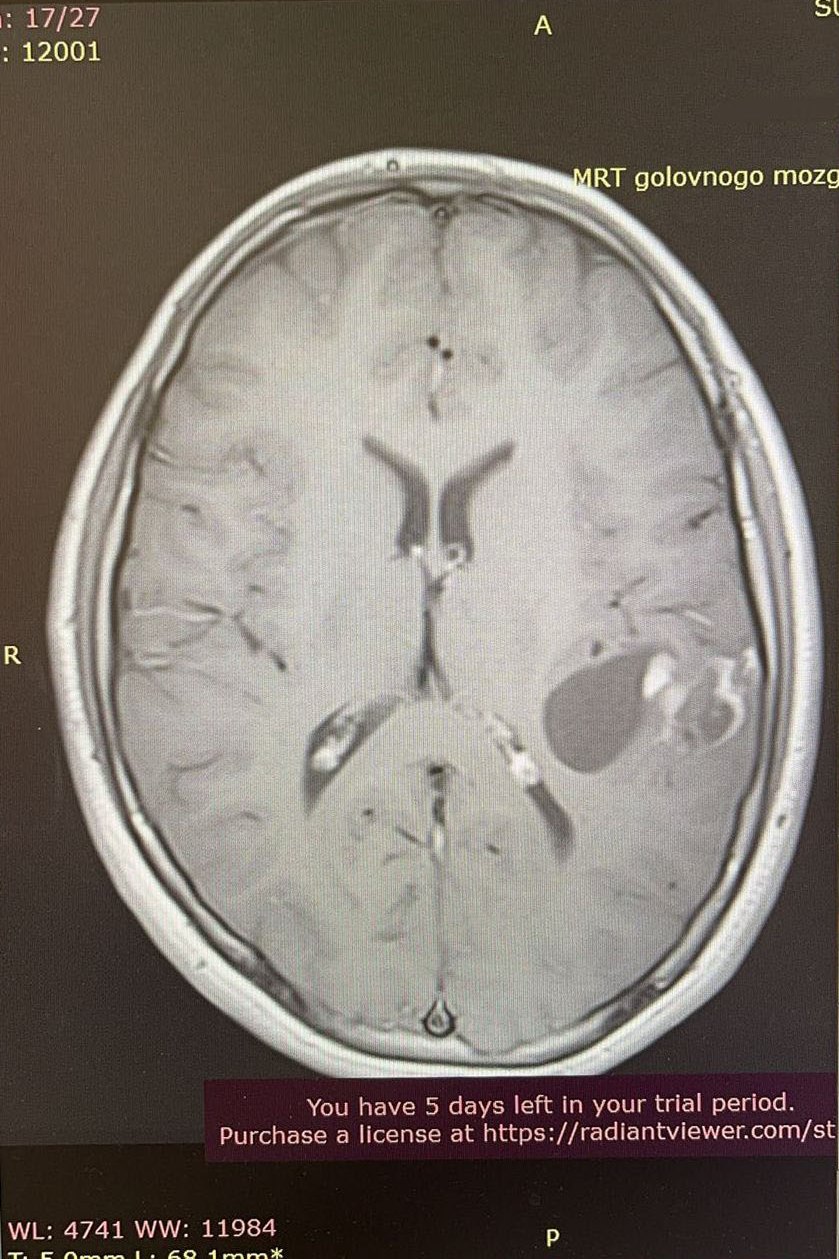 |
 |
| MRI before surgery | |
This location of the tumor is rare, and surgical treatment is associated with the risk of damage to one of the main functions of the brain. Therefore, it was decided to send the guy to Almazov Centre in St. Petersburg.
The patient underwent a thorough examination before surgery, and it was decided that he should be brought out of anesthesia directly during the surgery in order to exactly locate the speech area of the cortex relative to the tumor.
Intraoperative speech mapping is successfully performed for adult patients in many surgical centres of Russia but using this procedure for children requires an accurate selection algorithm.
“Along with certain physical inconvenience, the boy will need to sustain attention for a long time and make strong-willed efforts to properly complete tasks. Therefore, intraoperative mapping in awake surgery is available to pediatric patients with preserved personal identity and intellectual capacity. The neuropsychologist's task is to conduct a neuropsychological examination before surgery, psychologically prepare the patient for awakening in the operating room, and create an optimal setting for the speech tests. During the surgery, a neuropsychologist should maintain a constant verbal contact with the patient and assess the dynamics of the neuropsychological status after the procedure,” notes neuropsychologist Olga Shmeleva.
The patient’s attending doctor, Oleg Don, had a conversation with the boy and his mother. The neurosurgeon explained in detail the course of the procedure, the possibilities and necessity of neurophysiological control of the speech area of the cortex with the awakening, as well as all the potential risks of the surgery.
“During the surgical stage, brain functions can only be assessed using neurofunctional monitoring, when we apply current stimulation and immediately receive a response (we can see impulses on the screen). This way you can determine the functionality of the part of the brain controlling, for example, the muscle movement of the leg or arm. Unfortunately, speech cannot be tested unless the patient is awake during surgery. The absolute indication for awake surgery is speech mapping,” explains the operating surgeon, Head of Pediatric Neurosurgery Department at Polenov Neurosurgical Institute, Alexander Kim.
After all the preparatory stages, the specialists of Almazov Centre opted for awake brain surgery to remove the tumor in this patient.
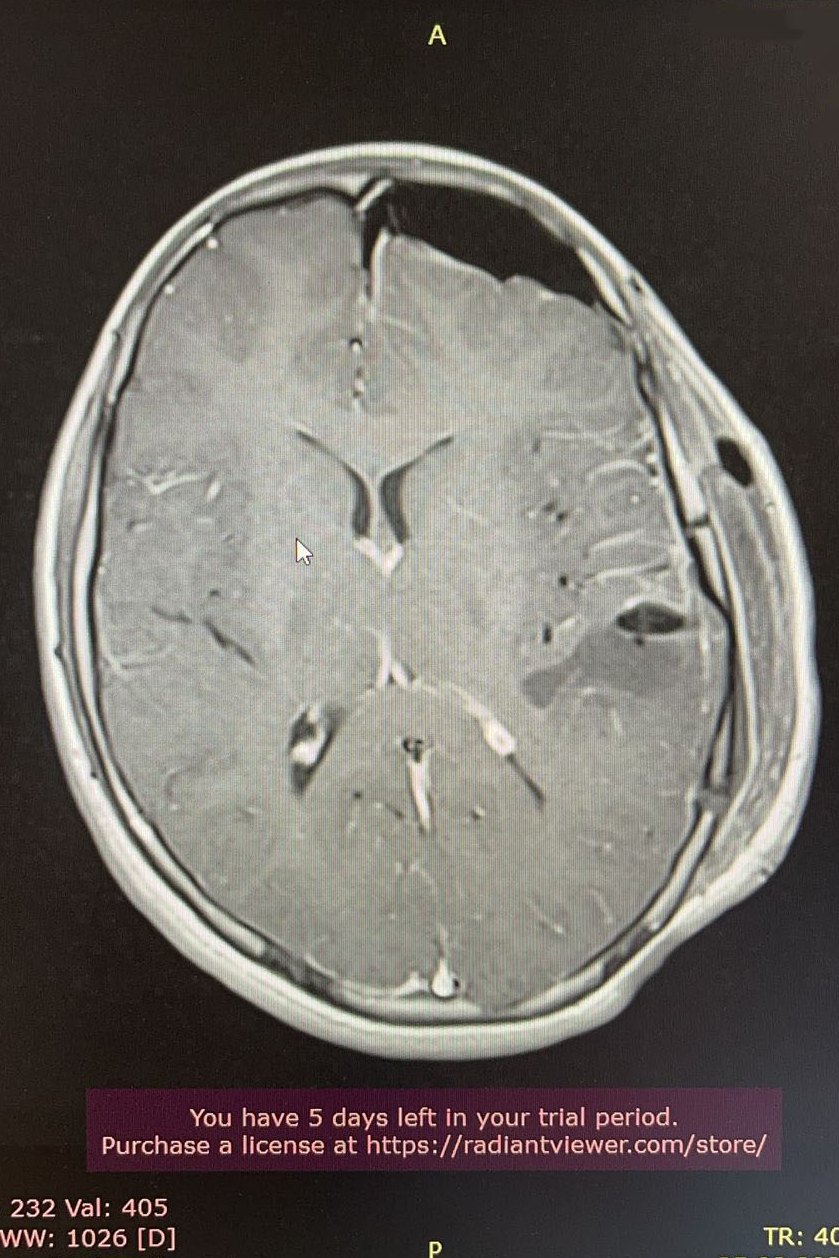
At the beginning of the procedure, the patient was put under general anesthesia. After trepanation and dura mater incision, the location of the tumor was determined by ultrasound, and then the patient was woken up from anesthesia. Speech areas of the brain were marked with numbers (mapping was performed), then they were stimulated, while the response was checked immediately.

Brain mapping
While the surgeon stimulated the brain areas, the neuropsychologist was constantly talking to the boy. During the entire removal procedure, specialists carefully monitored how the patient spoke, whether he confused words, checked his ability to use verbs and nouns. To check various functions of speech, he was asked to name the images in the pictures, to count, to give his last name, and so on.

When the surgeon came close to the speech area, serious changes in speech occurred.
“We realized that amnestic visual aphasia had set in – the patient continued to speak and comprehend, but was not able to recall the names of the objects in the pictures. For example, when he saw a picture of a tennis racket, he said that it was an object for playing tennis… This made us immediately stop and not touch this area. As soon as this was done, the speech function returned to normal,” said Artem Paltsev, Head of Neurosurgery Department, who attended in the operating room.

The multidisciplinary team of doctors also included PhD of the Medical Education Institute Dmitry Nizolin and neurophysiologist Yulia Zueva.
Largely thanks to the well-coordinated teamwork, the surgery was a success. The postoperative MRI showed that the tumor was completely removed. On the first day after the surgery, the patient had minor transient seizures with symptoms similar to those experienced during the surgery (when he could not remember the names of objects) and mild hand numbness. But they quickly regressed.
 |
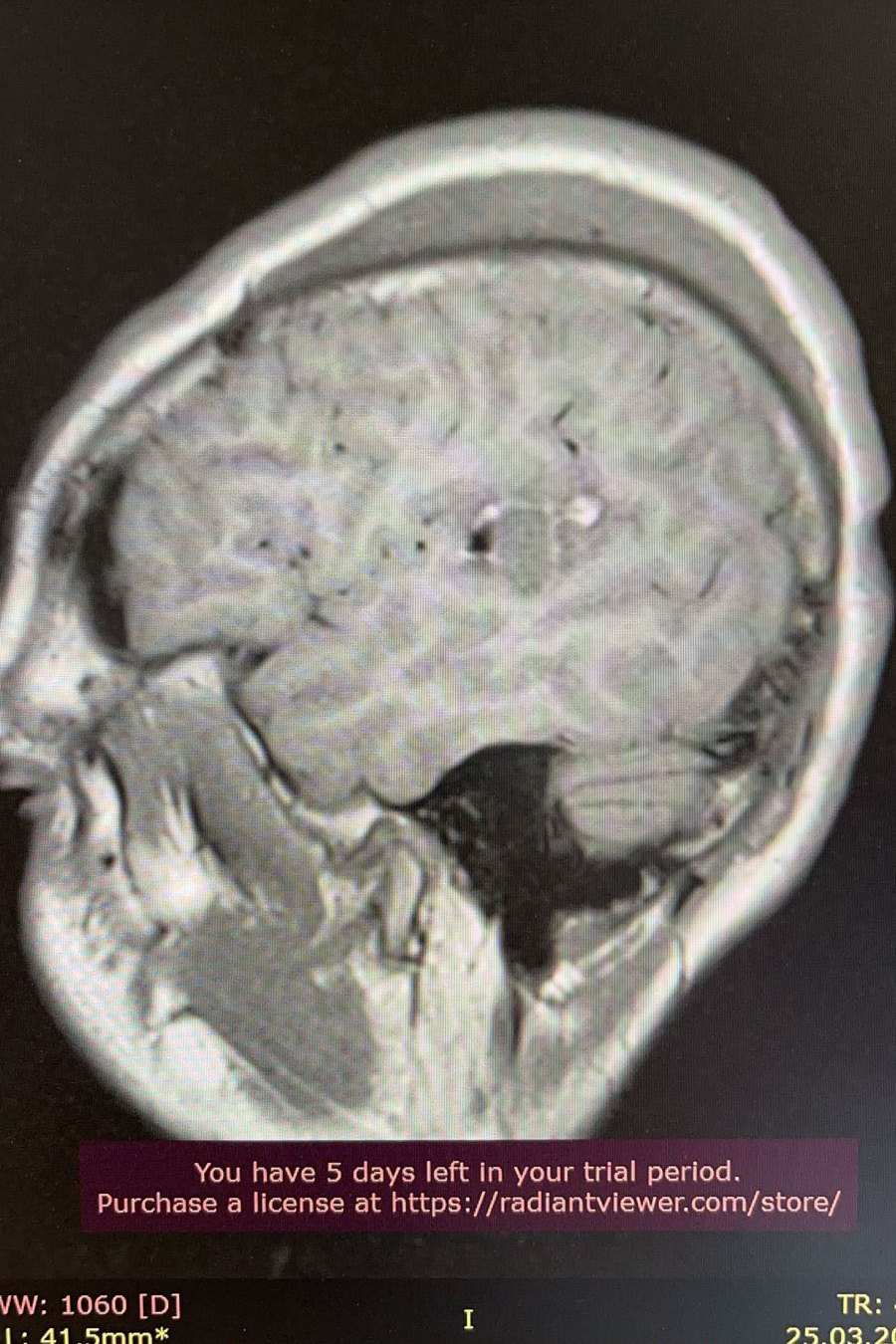 |
| MRI after surgery | |
Now the boy's condition is good, speech functions are fully preserved. In the future, he only should be monitored by a neurologist and undergo a follow-up examination every six months.

In the world, there are very few cases of using this technique in pediatric patients. Therefore, it is very important that specialists share such experiences with each other. After all, only after analyzing each clinical case of awake surgery, it is possible to assess and develop the optimal parameters of anesthesia as well as the stages of preparation and treatment procedure.
